UPMC Digital Pathology CME Courses
CME Credit Hours: 0.50
Target Audience:
Pathologists, Pathology Residents, Medical Students, Pathology Assistants and Pathology Assistant Students
Educational Objectives:
Upon completion of this activity, participants will be able to:
- As a result of participation in this activity, participants will be able to increase awareness of the pathologic evaluation of hematopoietic and lymphoid tissues
Additional Readings:
- Swerdlow S.H.C.E., Harris N.L., Jaffe E.S., Pileri S.A., Stein H., Thiele J., Arber D.A., Hasserjian R.P., Le Beau M.M., Orazi A., et al. WHO Classification of Tumours of Hematopoietic and Lymphoid Tissues. 4th ed. International Agency for Research on Cancer (IARC); Lyon, France: 2017.
- Foss HD, Anagnostopoulos I, Araujo I, Assaf C, Demel G, Kummer JA, Hummel M, Stein H. Anaplastic large-cell lymphomas of T-cell and null-cell phenotype express cytotoxic molecules.Blood.1996;88:4005-4011.
- Della Corte, C.M., Viscardi, G., Di Liello, R. et al. Role and targeting of anaplastic lymphoma kinase in cancer. Mol Cancer 17, 30 (2018).
- Touriol, Christian & Greenland, Catherine & Lamant, Laurence & Pulford, Karen & Bernard, Frederic & Rousset, Thérèse & Mason, David & Delsol, Georges. (2000). Further demonstration of the diversity of chromosomal changes involving 2p23 in ALK-positive lymphoma: 2 cases expressing ALK kinase fused to CLTCL (clathrin chain polypeptide-like). Blood. 95. 3204-7.
- Ruth H. Palmer, Emma Vernersson, Caroline Grabbe, Bengt Hallberg; Anaplastic lymphoma kinase: signaling in development and disease. Biochem J 15 June 2009; 420 (3): 345-361.
- Zhang Q, Ming J, Zhang S, Li B, Han X, Qiu X. Cytokeratin positivity in anaplastic large cell lymphoma: a potential diagnostic pitfall in misdiagnosis of metastatic carcinoma. Int J Clin Exp Pathol. 2013;6(4):798-801.
- Webb TR, Slavish J, George RE, et al. Anaplastic lymphoma kinase: role in cancer pathogenesis and small-molecule inhibitor development for therapy. Expert Rev Anticancer Ther. 2009;9(3):331?356.
- Azarova AM, Gautam G, George RE. Emerging importance of ALK in neuroblastoma. Semin Cancer Biol. 2011;21:267-275.
- Qiu Y, Li B, Zhang Y, et al. ALK-rearranged lung adenocarcinoma patient with development of severe sinus bradycardia after treatment with crizotinib: A case report. Medicine (Baltimore).2019;98(11):e14826.
- Lin JJ, Zhu VW, Schoenfeld AJ, et al. Brigatinib in Patients With Alectinib-Refractory ALK-Positive NSCLC. J Thorac Oncol. 2018;13(10):1530-1538.
Authors:
Davsheen Bedi, MD and Nidhi Aggarwal, MD
Release Date: 2022-06-14
Review Date: 2024-06-16
Expiration Date: 2025-06-17
No relationships with industry relevant to the content of this educational activity have been disclosed.
The University of Pittsburgh School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The University of Pittsburgh School of Medicine designates this enduring material for a maximum of 0.50 AMA PRA Category 1 CreditsTM. Each physician
should only claim credit commensurate with the extent of their participation in the activity.
Other health care professionals are awarded ( 0.05 ) continuing education units (CEU) which are equivalent to 0.50 contact hours.
Presenters for this program have been requested to identify financial or other relationships with manufacturer(s) of any commercial product(s) or with provider(s)
of any commercial service(s) which, in the context of their topics, could be perceived as real or apparent conflicts of interest.
The University of Pittsburgh is an affirmative action, equal opportunity institution.
Case 1059 - A Young Male with Abdominal Pain and a Para-spinal Mass
Contributed by: Davsheen Bedi, MD and Nidhi Aggarwal, MD
A maximum of 0.50 AMA PRA Category 1 Credits are available from a quiz on this case from the University of Pittsburgh's Internet-based Studies in Education and Research.
This course is eligible for the American Board of Pathology SAM credit
Click here to take the quiz and
earn 0.50 AMA PRA Category 1 Credits
Please review the case before taking the quiz. The site will now ask for your ABPath MOC number before taking the quiz if it was not supplied previously.
CLINICAL HISTORY
A Caucasian male in his twenties presented with a left abdominal pain and discomfort since a few weeks. There was no history of night sweats, fevers, or weight loss. CT scan of the abdomen revealed a 4.5 x 1.7 x 2.3 cm lobulated, non-vascular, soft tissue density on the left side of the aorta, below the level of the renal vessels. Initial radiologically guided fine needle aspiration (FNA) and biopsy were too small and non- representative. All serological markers for a germ cell neoplasm were negative and a scrotal ultrasound performed was unremarkable.
The patient presented again six years later with a left lower back pain, radiating down the left leg. CT scan performed revealed an increase in the size of the paraspinal mass to 10.1 x 6.5 cm (Figure 1A), with invasion into adjacent psoas muscle and enlargement of other peri-aortic lymph nodes. A CT guided biopsy performed showed sheets of large atypical cells with moderate pleomorphism, variably shaped nuclei, some with "horse-shoe shaped" nuclei and with abundant vacuolated cytoplasm (Figure 1B). Touch imprints prepared from the needle cores also showed these large atypical cells with bubbly vacuolated cytoplasm (Figure 1C). Some mitotic figures and multi-nucleated cells with prominent nucleoli were also noted.
On immunohistochemistry, the tumor cells were weakly positive for Leucocyte Common Antigen (LCA) (Figure 2A) and negative for both CD20 (Figure 2B) and CD3 (Figure 2C). In order to rule out a carcinoma, several keratin immunostains were performed, i.e. pan keratin, CK7, CK20, AE1/AE3 and CAM 5.2 of which all were negative, except for CAM5.2 which was weakly positive in some of the large atypical cells (Figure 2D). EMA (Figure 3A) and CD30 (Figure 3B) were also positive in the large atypical cells. ALK immunostain performed showed strong, diffuse nuclear and cytoplasmic positivity in the tumor cells (Figure 3C). However, none of the immunostains for T-cells were positive, i.e. CD2, CD3, CD5, CD7, CD4, CD8 and CD43. While TIA (T-cell intracytoplasmic antigen) was also negative, granzyme showed positivity in the tumor cells (Figure 3D). Additional immunostains performed to rule out other possibilities like Hodgkin lymphoma (PAX5, OCT2, BOB1), histiocytic neoplasm (CD68), germ cell tumor (CD117, OCT3/4, SALL4), metastatic lung carcinoma (P40, TTF1), metastatic gastrointestinal carcinoma (CDX2), sarcoma (actin, myogenin, desmin), melanoma (SOX10, Melan, HMB45), nerve sheath tumor (S100), etc. were negative.
Molecular studies performed were positive for T cell rearrangement, raising concerns for T cell lineage even though the IHC markers were negative. Further, cytogenetic florescence in-situ hybridization (FISH) studies using break apart probe for ALK showed four copies of ALK gene, two of which were rearranged.
The patient did not have any other lymphadenopathy or bone marrow involvement.
Figure 1: A - CT scan image of para-spinal mass measuring 10.1 cm x 6.45 cm, B - Photomicrograph of the needle core biopsy of the mass showing large atypical cells with vacuolated cytoplasm and some horse shoe shaped/ kidney shaped nuclei (black arrow heads) with prominent nucleoli, mitotic figures also present (black arrows) (400X, Hematoxylin and Eosin), C - Touch imprints from the needle core biopsy demonstrating the large atypical cells with vacuolated bubbly cytoplasm (200X, Diff Quick)
Figure 2: A - Weak positive staining in tumor cells with Leukocyte Common Antigen immunostain (200X, LCA IHC), B - Tumor cells negative for CD20 immunostain (200X, CD20 IHC), C - Tumor cells negative for CD3 immunostain, small T cells are positive (200X, CD3 IHC), D - Weak positive staining in some of the large tumor cells with CAM5.2 immunostain (200X, CAM5.2 IHC)
Figure 3: A - Tumor cells positive for Epithelial Membrane Antigen immunostain (200X, EMA IHC), B - Tumor cells positive for CD30 immunostain (200X, CD30 IHC), C - Tumor cells diffusely and strongly positive for nuclear and cytoplasmic Anaplastic Lymphoma Kinase immunostain (200X, ALK IHC), D - Tumor cells are diffusely positive for Granzyme immunostain (200X, Granzyme IHC)
 Figure 1 |
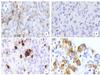 Figure 2 |
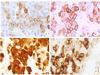 Figure 3 |
Please click the "Final Diagnosis" tab at the top of the screen to view the rest of the case.
FINAL DIAGNOSIS
Anaplastic Lymphoma Kinase positive Anaplastic Large Cell Lymphoma (ALK+ ALCL)
DISCUSSION
ALK positive Anaplastic Large Cell Lymphoma is a T-cell lymphoma that consists of large, pleomorphic, CD30+ T-cells that have abundant cytoplasm and horse-shoe shaped nuclei. These cells express the ALK protein and show chromosomal translocation involving the ALK gene.
ALK+ ALCL accounts for 3% of non-Hodgkin lymphoma in adults and about 20-30% lymphomas in children (1). It is seen more commonly in males and usually in the first three decades of life (1). It can involve both lymph nodes and extra-nodal sites, and clinically patients with ALK+ ALCL present with advanced stage disease usually.
Morphologically, these lymphomas are characterized by the hallmark cells i.e. large cells with horse-shoe shaped or kidney shaped nuclei, with prominent nucleoli and abundant amount of vacuolated to eosinophilic cytoplasm. There are various morphological patterns of ALK+ ALCL, namely the common pattern (60%), lympho-histiocytic pattern (10%), small-cell pattern (5-10%), Hodgkin-like pattern (3%) and composite pattern (15%) where more than one patterns can be seen in a single lymph node (1).
Immunohistochemically, these tumor cells are positive for CD30, EMA and ALK. The pattern of ALK staining can vary depending on the type of translocation the tumor harbors and will be mentioned subsequently. Most ALK+ ALCLs express one or more T cell markers. While CD3 is negative in >75% of the cases, CD2, CD5 and CD4 are positive in about 70% cases (1). Most cases are also positive for cytotoxic antigens like TIA1, Granzyme B and/or perforin.
Some cases of the ALK+ ALCLs may not be positive for any T-cell markers but show T-cell rearrangements at the genetic or molecular level. Such cases are called Null cell ALK+ ALCLs (2).
The most frequently occurring genetic alteration in ALK+ ALCLs is the translocation t(2;5)(p23;q35), between the ALK gene on chromosome 2 and the NPM1 gene on chromosome 5. The NPM-ALK chimeric protein is constitutively expressed from the NPM promoter, leading to the overexpression of the ALK catalytic domain and thus tumorigenesis. Many other varying rearrangements involving the ALK gene have recently been shown to be associated with ALCL, including ALO17-ALK, TRK-fused gene (TFG)-ALK, moesin (MSN)-ALK, Tropomyosin 3 (TPM3)-ALK, Tropomyosin 4 (TPM4)-ALK, ATIC-ALK, myosin 9(MYH9)-ALK and CLTC-ALK (3). While the NPM-ALK mutation causes a diffuse cytoplasmic and nuclear staining pattern for ALK, the TPM3-ALK results in a cytoplasmic ALK+ staining with membranous/ peripheral intensification (1) and the CTCL-ALK rearrangement results in a granular cytoplasmic staining (4). Most other translocations cause a cytoplasmic ALK staining. Therefore, strong nuclear and cytoplasmic ALK staining is to some extent indicative of the ALK-NPM1 translocation which can be confirmed on FISH studies using break apart probe or by genetic studies.
Amongst the important differential diagnoses of ALK+ ALCLs are the ALK+ Large B cell lymphomas, ALK+ systemic histiocytosis, inflammatory myofibroblastic tumor (IMT) and metastatic carcinoma. ALK+ Large B cell lymphomas are positive for B cell markers like CD20, PAX5, are usually CD30 negative and are more commonly associated with CTCL-ALK translocation that results in the granular cytoplasmic staining and not the nuclear ALK staining seen in ALK+ T-cell ALCL with NPM1-ALK translocation. ALK+ histiocytosis is also CD30 negative and shows expression for histiocytes markers like CD68. ALK fusions seen in IMTs are varied like TPM3-ALK, TPM4-ALK, CLTC-ALK , ATIC-ALK , CARS-ALK, RANBP2-ALK, SEC31L1-ALK (5). Inflammatory myofibroblastic tumors can be differentiated by a more commonly seen cytoplasmic ALK+ staining, and rarely nuclear membrane ALK+ staining in cases with RANBP2-ALK fusion. Metastatic carcinomas are usually positive for a number of keratins and also positive for the site specific primary tumor markers, whereas ALCLs are usually positive for EMA (1,6). Keratin positivity in lymphomas can be a common diagnostic pitfall and diagnosis is made based of various clinical, radiological and morphological findings and a battery of immunohistochemical stains (6). ALK gene has been found to play a role in several carcinomas. Esophageal squamous cell carcinoma harbors TPM4-ALK fusion, whereas lung adenocarcinomas are known to harbor ALK translocation with more than 19 different fusion partners, including EML4, KIF5B, KLC1, and TPR (7-9). Other ALK positive carcinomas include breast cancer (ELM4-ALK fusion in 2.4% cases), colon cancer (ELM4-ALK fusion in 2.5% cases), thyroid carcinoma (point mutations in exon 23 of the ALK gene, seen in 11% cases), renal cell carcinoma (VCL-ALK fusion, seen in pediatric RCCs) and neuroblastomas (ALK gene point mutations) (3,7-9). Many of these carcinomas can be ruled out based on the clinical history, thorough radiological and clinical examination to rule out other primary sites and on further confirmation with the site specific immunohistochemical stains as was also done in the present case as detailed earlier.
Our present case is an ALK+ ALCL with the characteristic NPM1-ALK fusion. It shows the characteristic strong nuclear and cytoplasmic staining for ALK immunostaining and the FISH studies confirmed the presence of ALK rearrangement based on break apart probe. Though, the partner gene cannot be determined with the break apart probe on FISH analysis, we could infer the partner gene to be NPM1 based on the strong diffuse nuclear and cytoplasmic ALK staining, which is not seen with any other ALK fusions.
There has been recently great interest in ALK related targeted immunotherapy. ALK fusion proteins and the constitutive ALK tyrosine kinase activity represent a therapeutic target in many malignancies with ALK rearrangement. Since ALK is not widely expressed in adult tissue, few toxic effects might be expected from treatment aimed at blocking ALK function (8). ALK small-molecule inhibitor compounds have demonstrated extremely robust anti-tumor efficacy in various trials. Crizotinib is one such small molecule inhibitor that is an FDA approved drug for ALK+ lung cancers. Brigatinib is used in patients who are intolerant to Crizotinib. Many other trials are undergoing for various ALK+ tumors (9,10).
The patient was started on chemotherapy including Cyclophosphamide, Hydroxydaunorubicin, Prednisone and Brentuximab, and after 5 cycles the size of the tumor reduced from 10.1 x 6.5cm to 4.6 x 3.4 cm. The patient is doing well except for the common side effects of nausea, vomiting which also resolved after the first 2 cycles.
Click here to take the quiz and
earn 0.50 AMA PRA Category 1 Credits
Please review the case before taking the quiz. The site will now ask for your ABPath MOC number before taking the quiz if it was not supplied previously.