UPMC Digital Pathology CME Courses
CME Credit Hours: 0.50
Target Audience:
Pathologists, Pathology Residents, Medical Students, Pathology Assistants and Pathology Assistant Students
Educational Objectives:
Upon completion of this activity, participants will be able to:
- Increase awareness of the histologic and immunohistochemical features of clear cell carcinoma (CCC) of the ovary
- Understand the molecular aspects of CCC
- Understand the treatment options and prognosis of CCC
Additional Readings:
- Gynecol Oncol. 2008;109:370-6
- 2. Clement PB, Young RH. Atlas of Gynecologic Surgical Pathology. Third Edition
- Am J Surg Pathol. 2009 Jan;33(1):14-21
- Virch Arch. 460:77-87 2012
- J Pathol. 2017 Oct;243(2):230-241
- Genes Chromosome Cancer. 2017 Oct 16 (Epub ahead of print). PMID: 29044863
- Histopathology. 2015 May;66(6):808-15
- Gynecol Oncol. 2017 Dec 9. pii: S0090-8258(17)31552-4
- Future Oncol. 2015;11(9):1389-405
- Appl Immunohistochem Mol Morphol. 2002;10:332–338
- Mod Pathol. 2000 Sep;13(9):962-72.
Authors:
Min Han, MD, PhD and Rohit Bhargava, MD
Release Date: 2018-06-30
Review Date: 2018-06-30
Expiration Date: 2021-06-30
No relationships with industry relevant to the content of this educational activity have been disclosed.
The University of Pittsburgh School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The University of Pittsburgh School of Medicine designates this enduring material for a maximum of 0.50 AMA PRA Category 1 CreditsTM. Each physician
should only claim credit commensurate with the extent of their participation in the activity.
Other health care professionals are awarded ( 0.05 ) continuing education units (CEU) which are equivalent to 0.50 contact hours.
Presenters for this program have been requested to identify financial or other relationships with manufacturer(s) of any commercial product(s) or with provider(s)
of any commercial service(s) which, in the context of their topics, could be perceived as real or apparent conflicts of interest.
The University of Pittsburgh is an affirmative action, equal opportunity institution.
Case 959-- A Post-Menopausal Female with an Ovarian Mass
Contributed by: Min Han, MD, PhD and Rohit Bhargava, MD
A maximum of 0.50 AMA PRA Category 1 Credits are available from a quiz on this case from the University of Pittsburgh's Internet-based Studies in Education and Research.
This course is eligible for the American Board of Pathology SAM credit
Click here to take the quiz and
earn 0.50 AMA PRA Category 1 Credits
Please review the case before taking the quiz. The site will now ask for your ABPath MOC number before taking the quiz if it was not supplied previously.
CLINICAL HISTORY
A postmenopausal woman in her 70s presented to the emergency room with abdominal pain. Physical examination revealed a non-mobile, non-tender right pelvic mass. Ultrasound found a large right ovarian mass, measuring about 9.2 x 7.6 x 7.2 cm. CA-125 was elevated at 42 (ref 0-20). Her past medical history was not contributory. The patient reported neither vaginal bleeding nor discharge. A total abdominal hysterectomy, bilateral salpingo-oophorectomy, lymphadenectomy and omentectomy were performed.
GROSS DESCRIPTION
The right tubo-ovarian complex weighed 416.9 g, which consisted of an enlarged ovary and an unremarkable fallopian tube. The ovary was entirely replaced by a 10 x 9 x 8.5 cm, tan, solid mass with areas of hemorrhage. The outer surface was smooth. The left adnexa and uterus were unremarkable.
HISTOLOGIC EVALUATION
Microscopically, the tumor demonstrated admixed tubulocystic and papillary growth patterns with hyalinized stroma. Most tumor cells had abundant clear cytoplasm with enlarged nuclei, irregular nuclear membrane and conspicuous nucleoli. In areas with abundant stroma, the tumor grew in variably-sized cysts and glands lined by cuboidal to flat cells with moderate atypia. Mitotic count was 5/10 HPF. The tumor cells showed strong and diffuse nuclear positivity for HNF-1 beta and Pax-8 by immunohistochemistry. CK7+ was also positive. CK20 and ER were negative.
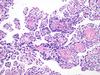 Fig1 |
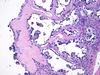 Fig2 |
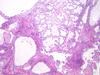 Fig 3 |
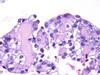 Fig 4 |
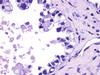 Fig 5 |
 Fig 6 |
Please click the "Final Diagnosis" tab at the top of the screen to view the rest of the case.
FINAL DIAGNOSIS
Clear Cell Carcinoma of the Ovary
DISCUSSION
Clear cell carcinoma (CCC) is an uncommon type of ovarian malignancy. Among the ovarian surface epithelial-stromal tumor category, the incidence of CCC was 4.8% in Whites, 3.1% in Blacks, and 11.1% Asians (1). Clear cell carcinoma can also occur in the endometrium and uterine cervix with similar morphology as their ovarian counterpart. In contrast to CCC of endometrium and cervix, CCC of the ovary frequently shows background of endometriosis or atypical endometriosis. Some cases of CCC of the ovary (especially without background of endometriosis) show adenofibromatous growth pattern.
Clear cell carcinoma has a variety of patterns, often admixed, including tubulocystic, papillary, and solid. The papillae tend to lack the hierarchical branching and prominent nuclear stratification of serous carcinomas, and often have distinctive cores (2). The cores of the papillae are often hyalinized, contain colloid-like material, or appear hollow. Clear cells and hobnail cells are the most common cell types. The clear cells (which are glycogen rich) are rounded or polyhedral and have eccentric nuclei. The hobnail cells contain a bulbous, usually dark nucleus that protrudes into lumens. Flat or cuboidal cells lining small cysts are less common and often impart a deceptively benign appearance. A subset of tumor cells can have oxyphilic rather than clear cytoplasm. Rarely, the entire tumor is composed of cells with oxyphilic cytoplasm (oxyphilic clear cell carcinoma variant). Mitoses are usually less frequent (mean 3-4?mfs/10?hpf) in CCC than in serous or other high-grade ovarian carcinomas. Immunohistochemically, clear cell carcinoma is usually positive for HNF-1 beta (nuclear), Napsin A (cytoplasmic), CK7, Pax-8 and negative for CK20, ER and WT-1 (3). P53 is variable and reported to show strong positivity in up to 34% of endometrial CCC. Molecular studies have identified ARID1A and PIK3CA gene mutations in 60% and 40% of CCCs respectively, which appear to be early events in CCC carcinogenesis (4). A recently published study of the genetic landscape of CCC showed that endometrial CCC constitutes a histologically and genetically heterogeneous group of tumors with varying outcomes (5). A recent Japanese study identified the following genes to be most frequently mutated in ovarian CCC: ARID1A (66.7%), PIK3CA (50%), PPP2R1A (18.8%), and KRAS (16.7%) (6).
Clear cell carcinoma is notorious for having poor response to conventional platinum-based chemotherapy and high risk for recurrence. Primary treatment of ovarian CCC and CCC of the uterus involves surgery with a total abdominal hysterectomy, bilateral salpingo-oophorectomy and omentectomy. Lymphadenectomy adds important prognostic information. The prognosis is heavily related to tumor stage with a recent study showing 5-year survival of 92% in stage I disease and 31% in advanced stage (7).
Click here to take the quiz and
earn 0.50 AMA PRA Category 1 Credits
Please review the case before taking the quiz. The site will now ask for your ABPath MOC number before taking the quiz if it was not supplied previously.